
Leave A COMMENT after reading and remember to share.

United by Unique – Cope & Live, UNTH Foundation, Oncoclinics Deliver Unstoppable Hope in Enugu
The aim of the joint outreach was to reduce isolation, enhance emotional resilience, improve quality of life, and ensure no one faces the mental health burden of cancer alone. The event underscored the urgent need to incorporate mental health care into all aspects of cancer treatment for truly comprehensive support. Unaddressed negative emotions can exacerbate anxiety and depression, weaken coping mechanisms, and reduce overall resilience—making proactive intervention essential.

Restoring Hope: Long-Term Support for Plateau IDPs
The crisis facing displaced families extends far beyond mental health needs. Daily hardships—hunger, malnutrition, lack of clean water, inadequate shelter, lost livelihoods, ongoing fear of violence, and profound trauma—are fueling chronic stress, anxiety, despair, PTSD, depression, and grief, especially among children and widows.

Beating Loneliness One Step at a Time: Lessons from the Ozalla Mind and Body Outreach
Events like this Total Care Mind and Body Outreach show that targeted, community-led actions deliver tangible, lasting benefits: improved quality of life, delayed cognitive issues, reduced emotional distress, and a stronger foundation for healthy aging in Nigerian communities.

The Youth Revolution in Education – Starting with Mental Health
A crucial yet often overlooked aspect of this theme is mental health awareness and support within education. Today's young people face unprecedented pressures: intense academic expectations, social media scrutiny, economic instability, peer challenges, and global uncertainties. These factors contribute to alarming rises in anxiety, depression, and other

Strategic Discussion for Integration of Infectious Disease Services into the Total Care: Mind and Body Outreach Program
The Total Care Mind and Body initiative is a flagship joint program between Cope and Live Mental Health Awareness Foundation and UNTH Foundation. It is designed to deliver free, integrated physical and mental health services to vulnerable populations, with the pilot on 24th January giving special attention to elderly persons (60+ years) and retirees.

Event Report: Humanitarian Support Program For Survivors Of Recent Attacks In Mushere Community, Bokkos Lga, Plateau State
The program was facilitated by the Resource persons from African Services.
Cope and Live Mental Health Awareness Foundation participated in an observational and assessment capacity, with representation by the Plateau State Program Manager.

New Era for Mental Health in Plateau State: CALMHAF Appoints Amos Zingven Selkap as SPM
As State Program Manager, Mr. Selkap will oversee and expand the Foundation’s activities in Plateau State, collaborating closely with the national management team to deliver impactful mental health awareness campaigns, community outreach, support services, and sustainable development projects. His leadership will emphasize measurable outcomes, periodic progress reviews, and alignment with CALMHAF’s broader goals of prioritizing mental well-being and empowering vulnerable communities.

Empowering Change: Successful Capacity-Building Training Held in Enugu!
A major focus of the session was the review and discussion of our 2026 Action Plan. This plan reaffirms our core mission to:
Deliver preventive mental health care
Raise widespread awareness
Provide meaningful education
Offer compassionate support — especially to vulnerable populations
By adopting this proactive, problem-solving approach, we aim to:

Hope + Compassion: What We're Planning for World Cancer Day and Beyond
Through this collaboration, our planned interventions include:
Reducing stigma surrounding cancer through open conversations and education
Raising awareness and providing vital education on prevention, early detection, and treatment options
Offering comprehensive psychosocial and compassionate support for cancer patients and their families — including free mental health talks, assessments, and counseling sessions.

Empowering Educators & Learners: Insights from Mrs. Uzoamaka Nwachukwu on Sunrise FM
Teachers wear many hats — they are nurturers, caregivers, motivators, coaches, mentors, and creative minds shaping young futures every single day. Yet, they often face intense scrutiny, judgment, and criticism from parents and society at large.
These pressures can lead to serious mental health struggles, including:
Aggression
Seeing Them vs. Seeing You: The Empathy-Projection Trap
In relationships, work, therapy, or daily life, recognizing the difference between empathy and projection can transform how we connect with others. Empathy bridges gaps and deepens understanding; unchecked projection builds walls and creates distance. Mastering this distinction leads to more authentic, supportive, and meaningful relationships.
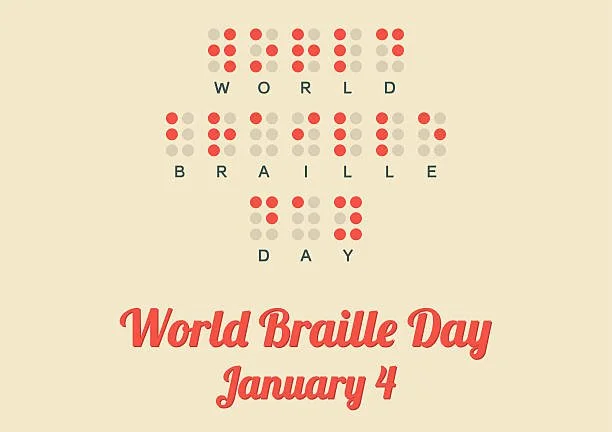
Braille and Mental Health: Touching the World Through Six Dots
Vision impairment significantly increases the risk of mental health challenges. Globally and in regions like Nigeria, blind and partially sighted individuals experience higher rates of depression, anxiety, social isolation, and reduced quality of life compared to sighted peers. Factors include loss of independence, dependency on others, stigma, and barriers to daily activities.
Braille literacy directly counters these risks by promoting autonomy and self-reliance—key protective factors against depression and anxiety. Studies show that proficient Braille users report higher self-esteem, confidence, life satisfaction, and emotional well-being.

Intentional Rest and Mental Health: A Vital Practice in a Busy World
Intentional rest is distinct from passive or unproductive downtime. Passive activities, while relaxing on the surface, often keep the brain stimulated through notifications, blue light from screens, or rumination, failing to provide deep recovery. For instance, scrolling social media or zoning out in front of the TV may feel like a break but can increase mental fatigue and prevent the nervous system from fully shifting into the parasympathetic "rest and digest" mode.

Moment Awareness Can Reduce Depression and Anxiety
Excessive mind-wandering correlates with increased negative emotions, including rumination (repetitive negative thinking about problems or feelings) and worry. These patterns are strongly linked to mental health challenges, such as depression and anxiety.
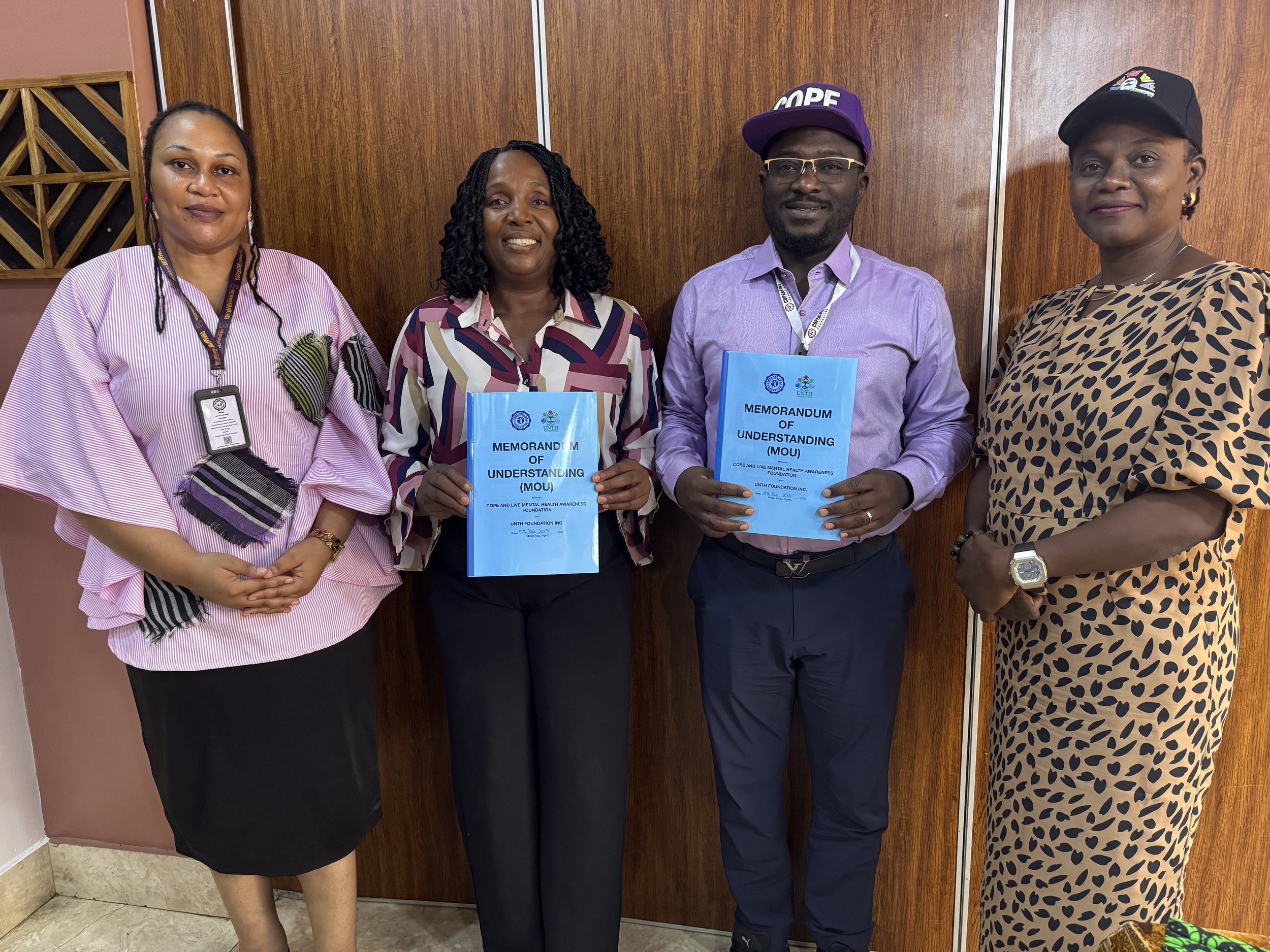
Total Care Mind and Body Initiative - Joint Problem Solving For Holistic Healthcare
The benefits of this collaboration extend far beyond the walls of the hospital and will have a transformative impact on Enugu State and the wider region through our joint “Total Care Mind and Body Initiative.” This initiative focuses on holistic support for communities, especially the underserved.
Designed as a joint proactive, problem-solving Initiative, it encourages early preventive steps and help-seeking behaviors, thereby reducing emergencies and medical costs.
Understanding Negative Self-Talk and Its Impact on Mental Health
Beliefs such as “I’m unlikeable” or “People will reject me” lead to withdrawal from relationships. The resulting loneliness reinforces the original negative belief, creating a self-perpetuating cycle.

How Fetal Alcohol Spectrum Disorders (FASD) Affect My Child’s Early Development and Mental Health
There is no known safe amount of alcohol during pregnancy, no safe trimester, and no safe type of drink. The only 100 % safe choice is to avoid alcohol completely when you are pregnant, planning to become pregnant, or breastfeeding.
If you drank alcohol before you knew you were pregnant, stop now – the baby’s brain continues to develop throughout pregnancy, and stopping at any time still helps.

Event Report: International Day of Persons with Disabilities (IDPD) 2025
Invited by the Yar'Adua Foundation, we were proudly represented by Mrs. Uzoamaka Nwachukwu, Co-Founder of the Cope and Live Mental Health Awareness Foundation. The gathering brought together government officials, disability rights advocates, NGOs, and community leaders in a shared commitment to building a truly inclusive Nigeria.

Puemperal Psychosis
This is a medical emergency. Quick action can save lives.
Never leave the mother alone, especially with the baby or anything sharp.
Gently take the baby away if she talks about harming the baby or herself.
Bring her to the nearest big hospital immediately or any hospital with a psychiatric unit).
If she refuses to go or becomes aggressive, call the emergency line 112 or the psychiatric emergency team.

Saying No Alone Does Not End Digital Violence Against Children And Teens
Quick summary checklist for parents:
Talk openly and often
Keep devices in family areas, especially at night
Use parental controls + monitoring appropriate to age
Teach “pause before posting” and “block + report”
Promise no over-punishment for coming to you
Doing even 3–4 of these steps dramatically reduces risk and harm. Digital violence against children is common, but it is largely preventable with proactive education and reasonable boundaries.